Screening for Lynch Syndrome
Ensuring people get screened for a common genetic condition called Lynch syndrome.
What are we trying to do?
Lynch syndrome is a common condition that can run in families and can lead to a higher risk of developing cancer at a younger age.
The most common types of cancers associated with Lynch syndrome are bowel cancer and womb cancer. Lynch syndrome is responsible for 3% of all bowel and womb cancer diagnoses. Other cancers related with Lynch syndrome are stomach, liver, pancreas, bladder, brain, and certain types of skin cancers.
We are leading a national project to ensure that more people are screened for Lynch syndrome across the UK meaning more cancers will be detected earlier.
Why is this important?
Data from 2018 estimates that 95% of people who have Lynch syndrome don’t know they have it.
Without a diagnosis, people with Lynch syndrome aren’t benefiting from regular monitoring which is essential for early detection and interventions that can reduce the risk of cancer.
It also means that their families are also not being screened for Lynch syndrome and won’t benefit from monitoring or treatment.
Listen to Emma as she shares her experience of being diagnosed with Lynch syndrome. Emma has been involved throughout this project sharing her vast knowledge and personal experiences and helping us to connect with more people who have Lynch syndrome.
Progress & next steps
95% of patients with bowel or womb cancers in England now get screened for Lynch syndrome compared to less than 50% before our work began.
We’ve supported NHS hospitals to offer standardised and equitable screening for Lynch syndrome for colorectal and endometrial cancer patients.
We’re monitoring and addressing any geographical variations in testing and supporting NHS Trusts to set up their own processes for screening and supporting their patients.
Who are we working with?
- Cancer Alliances across the South East
- Clinical Genetics teams
- North Thames Genomic Medicine Service
Learn more
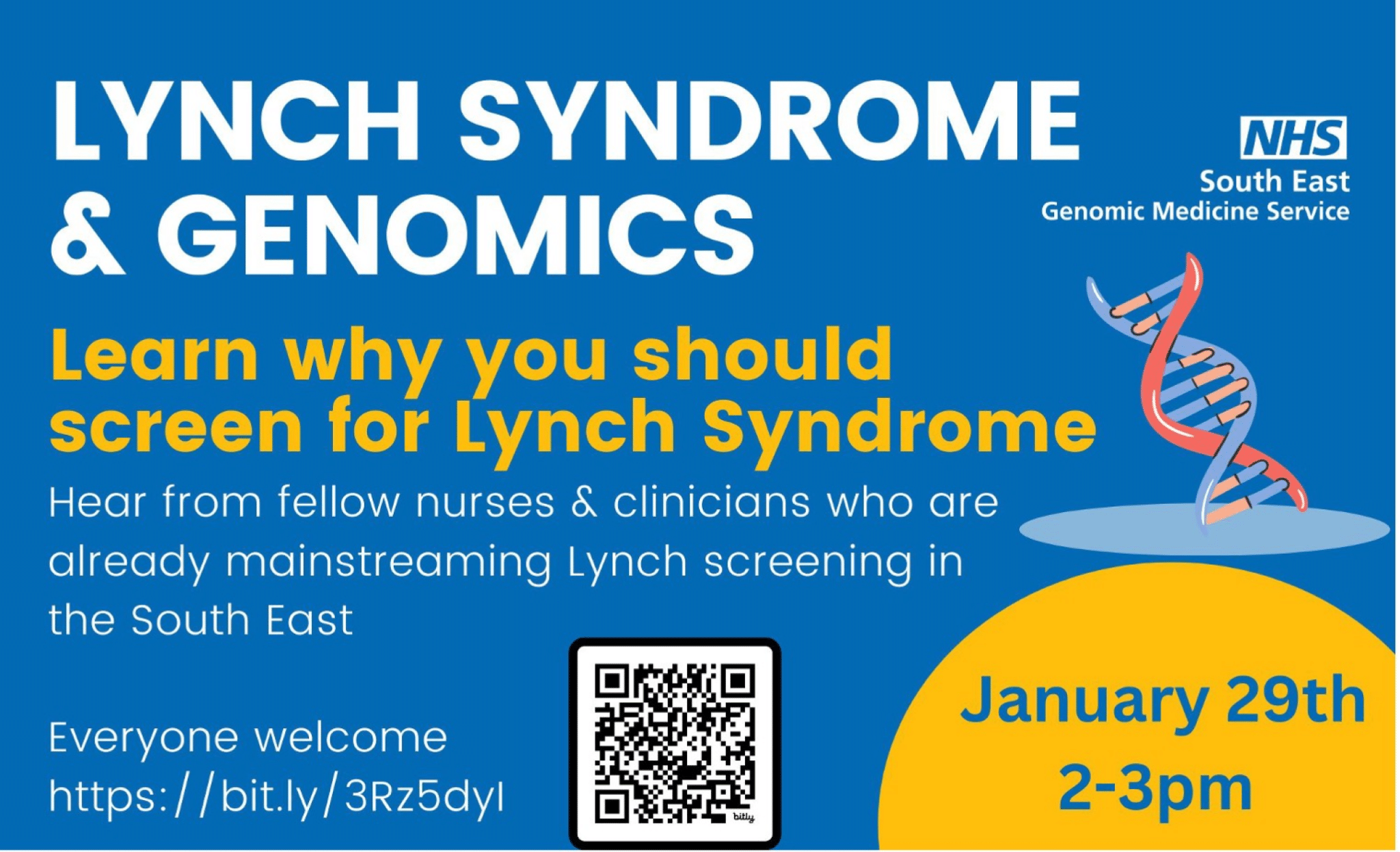
South East Regional Lynch Syndrome MDT meeting
We have a monthly MDT meeting for clinical discussion of Lynch syndrome cases. All clinicians who are delivering a mainstreaming service for Lynch syndrome are very welcome to join.
Every patient who has undergone germline testing will be discussed in the MDT regardless of their result (positive, negative, variant of unknown significance).
Please note, this MDT is for advice & guidance only.
For more information about the MDT and a copy of the MDT pro forma see below.
Resources
National guidance for implementing testing strategies:
- NICE Guidance [DG27]: Molecular testing strategies for Lynch syndrome in people with colorectal cancer
- NICE Guidance [DG42]: Testing strategies for Lynch syndrome in people with endometrial cancer
- NHSE handbook: Implementing Lynch syndrome testing and surveillance pathways
Additional guidance documents for healthcare professionals:
- NHS GMS Lynch Syndrome Transformation Project FAQs (Jan 2022)
- Guidance for healthcare professionals on accessing the NDRS Cancerstats2 dashboard for Lynch
Online training courses for healthcare professionals:
Your questions answered
Lynch Syndrome is caused by a genetic change in one of the DNA mismatch repair genes called MLH1, MSH2, MSH6 and PMS2. There is a fifth gene involved called the EPCAM gene because it turns off the neighbouring MSH2 gene. EPCAM alterations are very rare and only account for 6% of Lynch syndrome cases.
The function of DNA mismatch repair genes is to repair errors that may arise in the DNA code, which in turn protect people from developing cancer.
No. Lynch Syndrome does not always lead to or cause cancer, but the inherited genetic change that causes Lynch syndrome increases your risk of developing cancer to 80% over your lifetime.
The risk of developing cancer from Lynch Syndrome depends on which gene is affected. The risks associated with variants in PMS2 are much lower than the risks associated with variants in MLH1 for example.
If your patient has a strong family history of cancer then you should recommend they get referred to your regional Clinical Genetics team for a genetic assessment. This will delve deeper into their family history to assess their risk.
The term ‘mainstreaming’ refers to the shift of genomic testing away from Clinical Genetics into other clinics and specialities.
Within the Lynch Syndrome testing pathway, this means healthcare professionals in the oncology MDTs becoming directly involved in the consenting of patients for germline genetic testing, the requesting of the test and in communicating the result. A goal of this project is to upskill oncology MDTs to provide a mainstream testing service for Lynch Syndrome. This will help ensure all eligible patients receive germline testing without delay and results can effectively inform management.